The Origins of Interventional Uro-Radiology
Invaluable contributions to urological practice (by the Museum staff)
A specialty once regarded as carrying out dangerous, quirky & unjustified procedures has become a vital adjunct to every urological team
 Some urologists may recall being summoned from their beds in the early hours of the morning by a request to cannulate a vein urgently so that the patient could receive intravenous contrast for their emergency IVU. If that is a bitter memory, then spare a thought for the junior staff of William Barr Stirling (1914-1984; pictured below right) who were handed the task of cannulating the patient’s abdominal aorta to carry out an aortogram.
Some urologists may recall being summoned from their beds in the early hours of the morning by a request to cannulate a vein urgently so that the patient could receive intravenous contrast for their emergency IVU. If that is a bitter memory, then spare a thought for the junior staff of William Barr Stirling (1914-1984; pictured below right) who were handed the task of cannulating the patient’s abdominal aorta to carry out an aortogram.
 Lumbar aortography required a general anaesthetic and helped in the diagnosis of congenital abnormalities, cysts, tumours, hydronephrosis, stones, hypoplasia and renal tuberculosis. The procedure involved a general anaesthetic and a very long needle with a high-pressure hand-pump to deliver the contrast medium. Considerable skill was needed to get good images.
Lumbar aortography required a general anaesthetic and helped in the diagnosis of congenital abnormalities, cysts, tumours, hydronephrosis, stones, hypoplasia and renal tuberculosis. The procedure involved a general anaesthetic and a very long needle with a high-pressure hand-pump to deliver the contrast medium. Considerable skill was needed to get good images.
But that all changed in early 1953 when Sven-Ivar Seldinger, at the Karolinska Institutet in Sweden, carried out a procedure which his contemporaries had derided as "dangerous, quirky & unjustified". Using equipment of his own design (contemporary version pictured below), he inserted a small catheter into a patient's arterial system by puncturing the artery with a fine sheathed needle. He exchanged the needle for a guidewire passed down the sheath, removed the sheath and then fed a fine catheter over the guidewire into the artery to inject contrast medium (X-ray dye) after withdrawing the guidewire.
On that day, the Seldinger technique was born and the specialty of "Interventional Radiology (IR)" was, in effect, invented; Seldinger's technique is still used, almost unchanged, to this day.
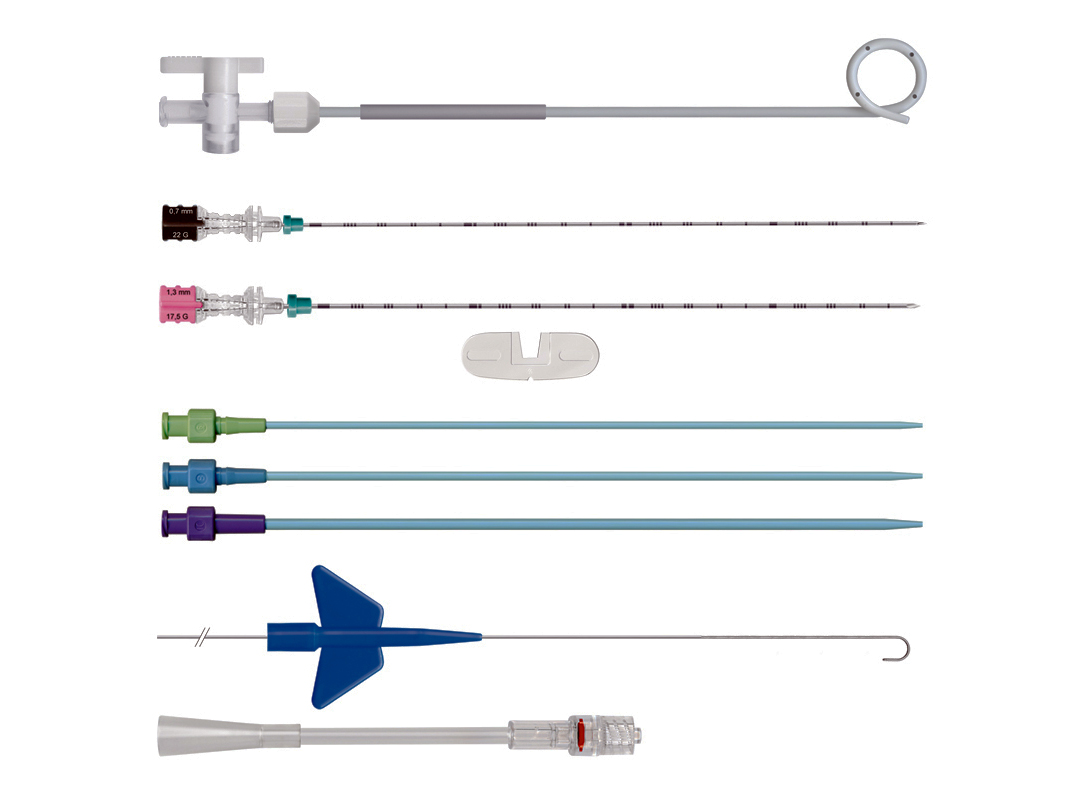
Contemporary Seldinger set - needles, sheaths, guide wire, pigtail catheter & connector
Fluoroscopy (X-ray screening) had been introduced in the 1920s, allowing radiologists to work with real-time imaging of internal structures to guide their interventions although, nowadays, ultrasound, computerised tomography (CT) and magnetic resonance imaging (MRI) are more likely to be used. However, it was not until the early 1960s that IR really began to "take off".
Charles Dotter (1920-1985), often called the "Father of Interventional Radiology", used fluoroscopy to perform the first angioplasty for a blocked artery in the leg on 16 January 1964 in Oregon. For almost 10 years, however, interventional radiology remained largely confined to vascular procedures - angioplasty, stenting & embolisation.
From 1972 onwards, non-vascular interventions were rapidly being introduced. Almost overnight, radiologists became skilled not only in diagnostics but also in therapeutic interventions - and they rapidly became a vital part of the clinical team.
Interventional radiology in urological practice
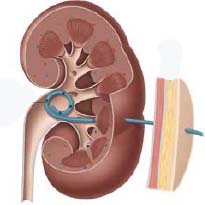
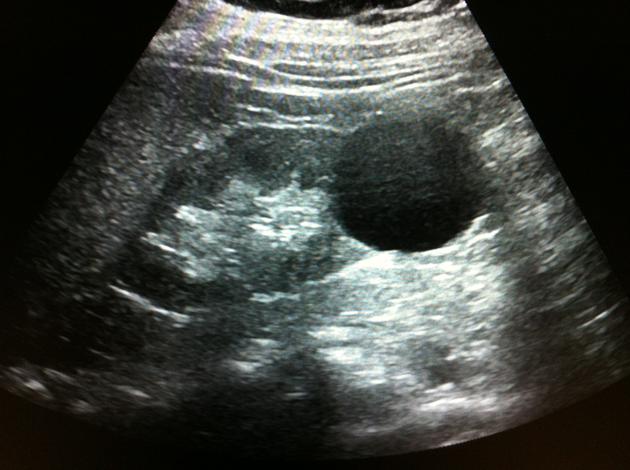 Initially, radiologists confined themselves to fine-needle aspiration (FNA) biopsies of suspicious lesions, emptying & sclerosing cysts in the kidney (pictured right), and draining collections of urine, pus or blood. However, as the design of catheters, stents and other devices progressed at pace, driven by the radiologists themselves, they expanded their expertise to more inventive levels.
Initially, radiologists confined themselves to fine-needle aspiration (FNA) biopsies of suspicious lesions, emptying & sclerosing cysts in the kidney (pictured right), and draining collections of urine, pus or blood. However, as the design of catheters, stents and other devices progressed at pace, driven by the radiologists themselves, they expanded their expertise to more inventive levels.
Percutaneous nephrostomy
Percutaneous nephrostomy has been the saviour of many a urologist & urological patient. Once access is established to the kidney, it has become possible to insert, change and remove ureteric stents, tubes etc. Stents for the ureter became commonplace during the 1980s. However, and more importantly, percutaneous nephrostomy has proved to be a "life-saver" in patients with septicaemia due to an infected kidney above an obstructed ureter.
It also became the initial step of percutaneous nephrolithotomy following which a tract was dilated into the kidney to allow stones to be removed under direct vision by a surgeon; and it was used in the 1980s to access the kidney for upper tract urodynamic (pressure-flow) studies by Bob Whitaker & Prof Tom Sherwood in Cambridge.
Interventional uro-oncology
This has progressed dramatically from simple FNA biopsy to image-controlled thermotherapy (heating), cryotherapy (freezing), radiofrequency/microwave ablation and ultrasound destruction of tumours in the urinary tract. New tools such as biodegradable stents, MRI/ultrasound fusion to guide prostate biopsies, and advanced embolic agents are constantly being developed.
Embolisation
Angiography, including Stirling's lumbar aortography, was used for some time to assess the vascular anatomy of tumours (especially in the kidney) but has now largely been superseded by advanced CT & MRI techniques to display tissue vasculature.
Arteriography & arterial embolisation are still used for tumours (either to stop bleeding or to minimise it during surgery), for refractory priapism or for uncontrolled bleeding from the urinary tract as a result of trauma - either from external violence or following surgery. Prostatic artery embolisation (PAE) is in general use as a non-invasive treatment for selected patients with benign prostatic obstruction.
Venography & venous occlusion, using plugging materials such as foam, coils & sponges, is often employed to treat varicoceles (see image below) and avoids the need for surgery with all its attendant risks. The complication rate is low and the procedure is both safe & effective in relieving symptoms, although probably not quite as effective as surgery.
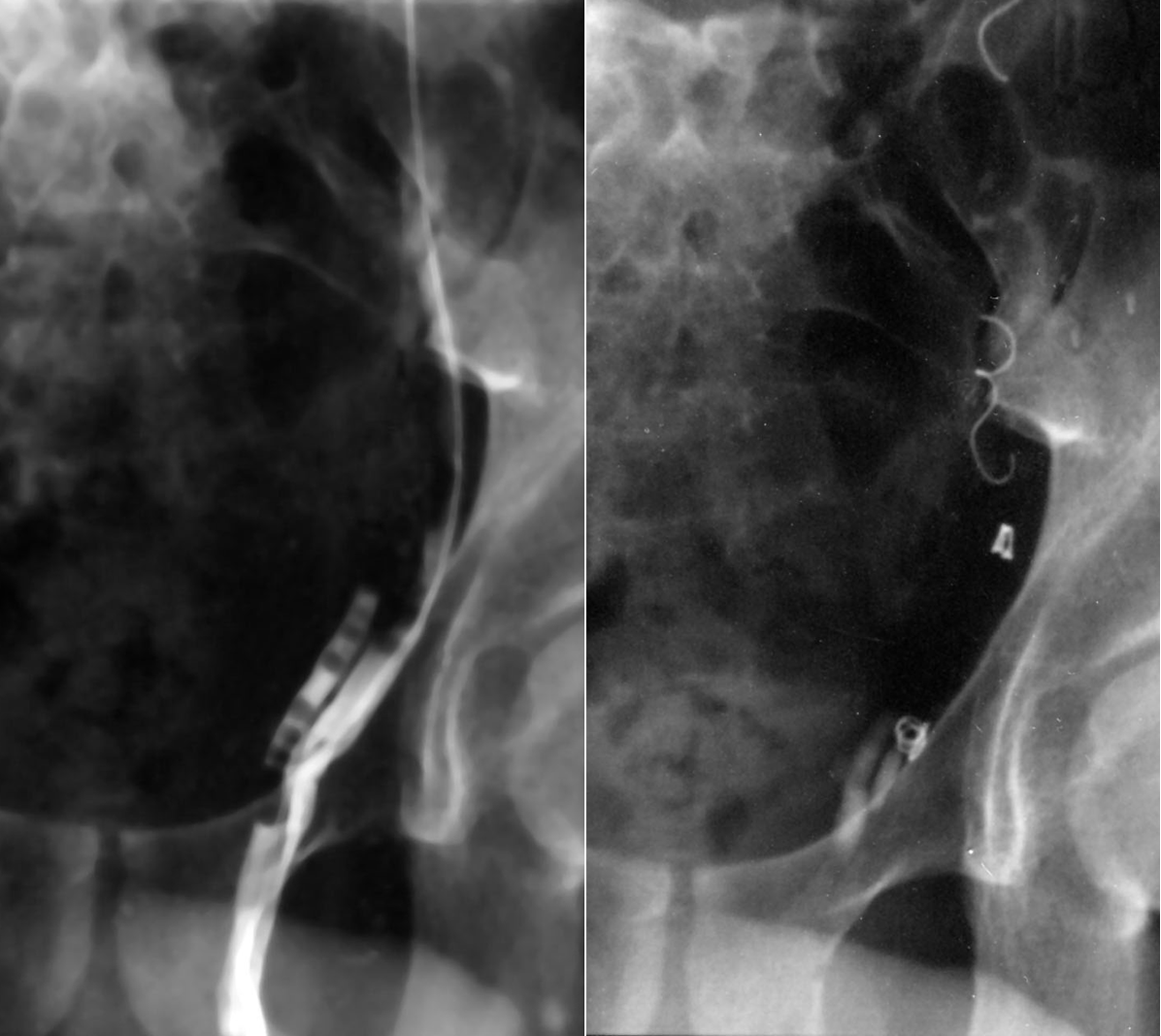
Before (L) & after (R) coil & sponge occlusion of a varicocele
(via a puncture of the right femoral vein)
Removing "stuck" urethral catheters
Finally, on a lighter note, every urologist must at some stage have been called to remove a self-retaining catheter in which the balloon cannot be deflated. Using a guidewire through the balloon channel to effect a puncture is often unsuccessful and over-inflating the balloon to burst it risks leaving catheter fragments in the bladder. However, with a simple ultrasound probe and a fine needle passed suprapubically, an interventional uroradiologist can puncture the balloon in just a few seconds ... problem solved!
The bottom line
The days of radiologists sitting in darkened rooms, talking to dictating machines & reporting on plain X-rays are long gone - radiologists are now vital & valued members of the urological team in both assessing & treating patients. In some areas, they have actually taken over the clinical management of certain conditions from urologists, resulting in minimisation of pain and a reduction in the physical trauma of surgery, as well as shortening hospital stays.
Additional information
Click on any link below to access more detailed information about items & individuals featured above, or click here to go to the main History section of this website for more general history content:
|
Charles Dotter
(pioneer of angioplasty)
|
High-Intensity Focussed
Ultrasound (HIFU)
|
Percutaneous
nephrostomy
|
|

Radiofrequency ablation
(RFA)
|

Society of Interventional
Radiology (SIR)
|

Sven-Ivar Seldinger
|
|

Ureteric stents
|

Bob Whitaker
|

William Barr Stirling
|
← Back to BAUS 80th Anniversary