Surgery for Benign Enlargement of the Prostate
The "silly operation" which became routine (by the Museum staff & Tom McNicholas, Stevenage)
From open surgery and several weeks in hospital to day-case laser surgery or relief of symptoms in an outpatient setting
 Transurethral resection of the prostate, TURP, is one of the operations that defines urology,but, although it was invented in 1927 - well before the formation of BAUS - it took some considerable time to be accepted in the UK. TURP is by no means a British operation; it is a citizen of America and its immigration into Great Britain was a tortuous one. Even before the Second World War, Terence Millin in 1932, wrote that there was a "strong feeling of distrust" in the UK regarding any transurethral prostatic surgery.
Transurethral resection of the prostate, TURP, is one of the operations that defines urology,but, although it was invented in 1927 - well before the formation of BAUS - it took some considerable time to be accepted in the UK. TURP is by no means a British operation; it is a citizen of America and its immigration into Great Britain was a tortuous one. Even before the Second World War, Terence Millin in 1932, wrote that there was a "strong feeling of distrust" in the UK regarding any transurethral prostatic surgery.
 Millin, of course, devised the open, retropubic, prostatic enucleation procedure. He published it in 1945, the year BAUS was formed. This relatively straightforward operation, which could be carried out by any competent general surgeon with no endoscopic skills, was one of the reasons TURP did not take off in the UK.
Millin, of course, devised the open, retropubic, prostatic enucleation procedure. He published it in 1945, the year BAUS was formed. This relatively straightforward operation, which could be carried out by any competent general surgeon with no endoscopic skills, was one of the reasons TURP did not take off in the UK.
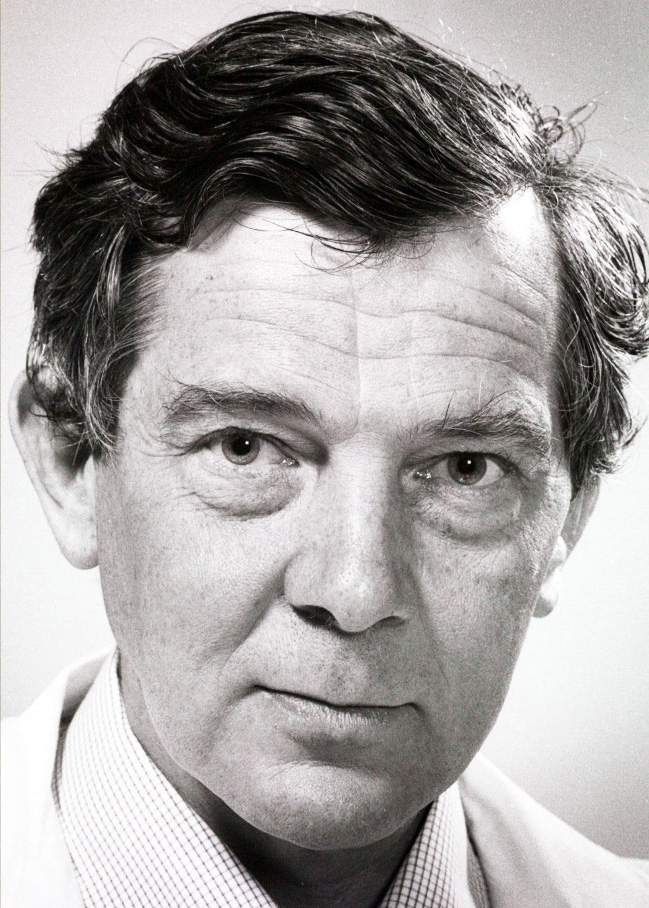
In 1960, John Blandy (1927–2011), then a Senior Registrar at the London Hospital, travelled to Chicago to get his "American experience’" in the hope of making himself a more attractive candidate for a consultant post in London. He learned the technique of TURP in both Chicago and Ann Arbor from Reed Nesbit, at that time the major US proponent of TURP. Convinced it was the right way to go, Blandy not only practised but also taught TURP to his trainees back in England. Even so, he was told by his senior colleagues at St Peter’s Urology Hospital, “We want you to give up that silly TURP operation John, it will bring St Peter’s into disrepute”. Blandy’s book, Transurethral Resection was first published in 1971. Writing the foreword for the 5th edition in 2005, he noted that, when it was first published, hardly any TURPs were being done in the UK.
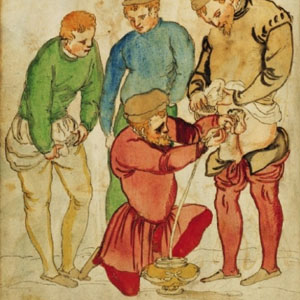
However, there was another group of British and Irish urologists who travelled to America to investigate transurethral prostatectomy; they brought back new skills and used them extensively. However, this skill was not TURP - this group of enthusiasts used the prostatic punch. The Punch Club was founded in 1949 by Tom Chapman (1903-1966), Henry Hamilton Stewart (1904–1970), John Swinney (1912–1988) and Tom Lane (1894–1967). Its first meeting was at the Meath Hospital in Ireland, Lane’s unit. These were the British and Irish urologists who promoted transurethral prostatic surgery and were extremely skilled in resecting large volumes of prostate tisssue.
Thompson/Swinney Punch

John Swinney's modification of the Gershom Thompson Punch
Disassembled Punch
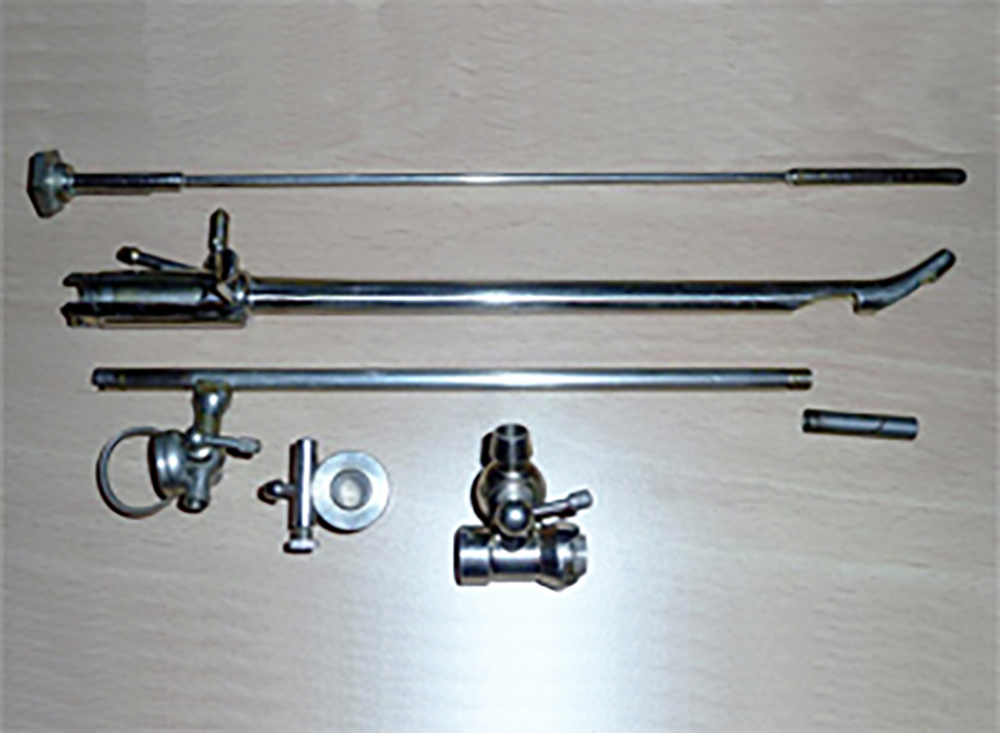
The punch disassembled showing the window into which the prostatic tissue falls to be cut off with the sliding blade
Millin Resectoscope
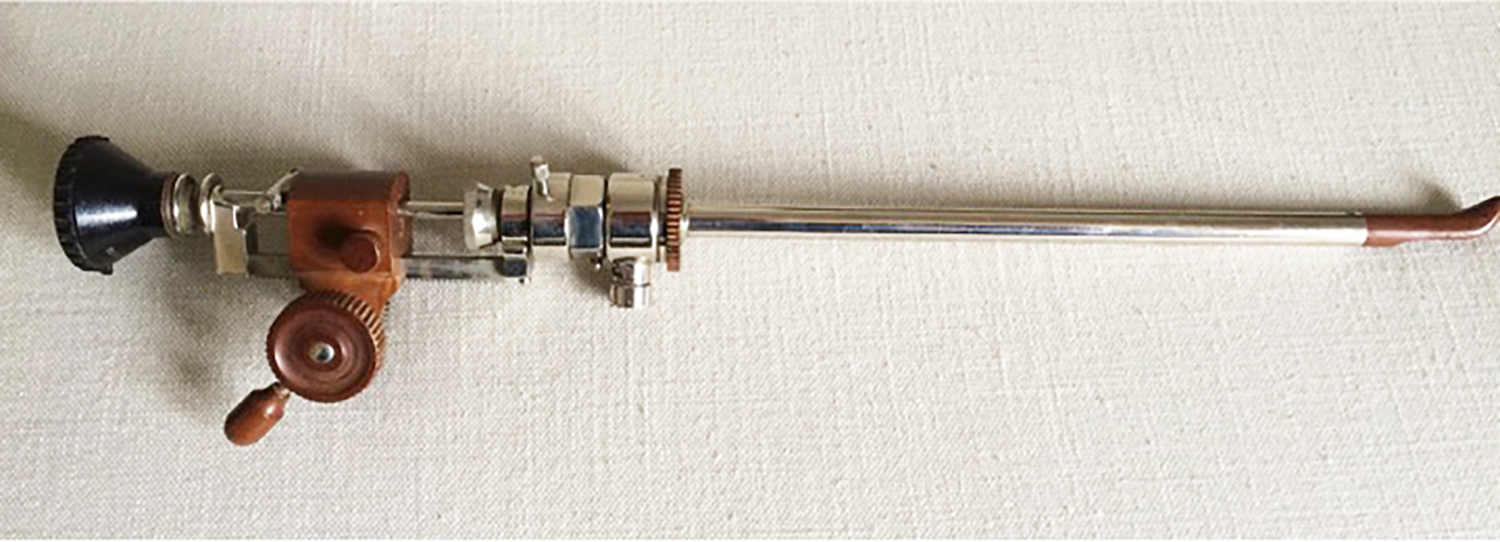
This is a Millin's resectoscope, based on the original McCarthy model. The loop is moved by a rack and pinion action, quite different from the sprung handle we use today.

 Probably the most important change in technology around this time, however, was the Hopkins rod lens system. Despite his enthusiasm for TURP, John Blandy wrote that he felt he was operating almost blind using the old bulb-lit telescopes. The invention of a brilliant optical scientist, Harold Hopkins, 1918–2001 (pictured left), the rod lens system increased light by a factor of 80 and, therefore, allowed the surgeon to see into the bloody world of the TURP. Due to the persistence of James Gow, 1917–2001 (pictured right) of Liverpool - another keen resectionist - Harold Hopkins redesigned the cystoscopic telescope and, with Karl Storz, 1911–1996), the German instrument maker, introduced the fibreoptic light source. This was the major boost that endoscopic surgery needed to bring it into the mainstream
Probably the most important change in technology around this time, however, was the Hopkins rod lens system. Despite his enthusiasm for TURP, John Blandy wrote that he felt he was operating almost blind using the old bulb-lit telescopes. The invention of a brilliant optical scientist, Harold Hopkins, 1918–2001 (pictured left), the rod lens system increased light by a factor of 80 and, therefore, allowed the surgeon to see into the bloody world of the TURP. Due to the persistence of James Gow, 1917–2001 (pictured right) of Liverpool - another keen resectionist - Harold Hopkins redesigned the cystoscopic telescope and, with Karl Storz, 1911–1996), the German instrument maker, introduced the fibreoptic light source. This was the major boost that endoscopic surgery needed to bring it into the mainstream
The number of TURPs performed in some centres, began to increase gradually. In James Gow’s 1973 series of 300 TURPs, it was the treatment of choice in 80% of enlarged prostates. At the London and St Peter’s, by 1978, 95% of prostatectomies were performed transurethrally. Even so, in a 1980 BMJ Editorial it was noted that 80% of prostatectomies were still being carried out by general surgeons, not urologists, and that most of these were still open Millin’s operations. Moreover, in hospitals who did not have a urologist (where prostatectomy was likely still being performed open), the mortality rate was 11.2% against the urologists' 2%.
 In reality, it was not until the end of the 20th century that general surgeons finally ceded the prostate to urologists. TURP can be a difficult operation to perform well, it is a difficult operation to learn, and one needs to be well-versed in the skills of cystoscopy before being let loose with an electrified loop within the lower urinary tract. It is - and always has been - an operation for the specialist. Improved light sources, better optics and use of video systems allowed better training of urologists and led to better outcomes, so that TURP eventually displaced the open Millin’s prostatectomy for all but the largest of prostates; open prostatectomy for BPH is rarely seen by today’s trainees.
In reality, it was not until the end of the 20th century that general surgeons finally ceded the prostate to urologists. TURP can be a difficult operation to perform well, it is a difficult operation to learn, and one needs to be well-versed in the skills of cystoscopy before being let loose with an electrified loop within the lower urinary tract. It is - and always has been - an operation for the specialist. Improved light sources, better optics and use of video systems allowed better training of urologists and led to better outcomes, so that TURP eventually displaced the open Millin’s prostatectomy for all but the largest of prostates; open prostatectomy for BPH is rarely seen by today’s trainees.
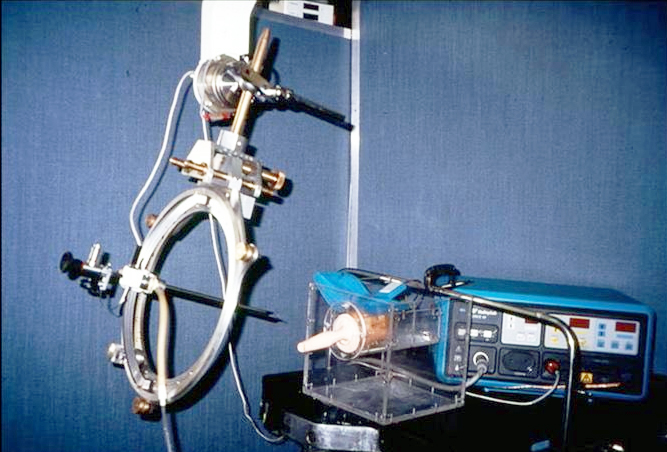
In April 1991, John Wickham performed the first fully robotic prostatectomy transurethrally using the Probot (pictured right) - a robotic device which operated a rotating blade within sheath after being pre-programmed with the dimensions of the prostate under treatment. This resulted in Wickham acquiring the title of "godfather" of robotics in urological surgery and it was probably he who first coined the term "minimally-invasive surgery".
The bottom line
Now the TURP is under fire again, this time from less complex treatments, as urologists continue to pursue the path of minimal invasion. The ingenuity of urologists and the support of Med-Tech companies has resulted in a veritable "tsunami" of devices to treat BPH being made available since the start of the 21st century.
However, BAUS urologists and their symptomatic male patients now have available the ultimate developments of the techniques of transurethral removal of the prostate for those who need it, with the addition of a wide range of safe, moderately effective, evidence-driven, “minimally invasive” surgical treatments for those with milder symptoms, or who wish to make informed choices to avoid specific side-effects.
Timeline of minimally-invasive interventions for BPH
| 1970s |
CRYOTHERAPY
Freezing the prostate with a transurethral probe was used by some in the 1970s & 80s but gave poor results and is no longer used in its original form. A more up-to-date version uses argon gas injected through probes into the prostate under transrectal ultrasound control but is only licensed for use in prostate cancer |
| 1970s & 80s |
BLADDER NECK INCISION
it soon became clear that, in men with small, obstructive prostates, a full resection of the prostate was not really necessary. A simple incision of the bladder neck, using an endoscopic spike (Colling's knife), was usually sufficient to give symptomatic relief with a low-risk of complications and preservation of antegrade ejaculation. It is still in use today, although now often performed using a laser. |
| 1980s |
TRANSURETHRAL MICROWAVE THERAPY (TUMT)
External heating of the prostate eventually causes the gland to shrink but involves expensive equipment. Although it provided relief of symptoms in the short & medium term, long-term results were unsatisfactory and it is no longer used |
| 1990s onwards |
LASER SURGERY - TULIP, ILC, HoLEP and GREENLIGHT ABLATION
Interstitial laser thermotherapy was popularised in the early 1990s by Tom McNicholas in Stevenage. It gave good, early results after a period of swelling, obstruction and inflammation, but it did not provide long-termm relief of symptoms. Popularised in New Zealand by Peter Gilling & Mark Fraundorfer, HoLEP provides very good, durable symptomatic relief, low risks, results in very effective enucleation and can be performed in high-risk patients, even those with clotting disorders or taking anticoagulants. Greenlight laser ablation uses laser energy to vaporise the prostate, rather than enucleating it, giving similar results to HoLEP. Generally, laser enucleation & vaporisation have now taken over the endoscopic management of BPH |
| 2000 onwards |
PROSTATE ARTERY EMBOLISATION (PAE)
First described by Margolies et al in the 1970's, PAE evolved from embolisation of the internal iliac arteries for severe lower urinary tract bleeding, often as a result of prostatic surgery. It causes shrinkage of the prostate and is used mainly for patients who are viewed as high-risk for any form of more invasive surgery |
| 2010 onwards |
UROLIFT ®
This technique was developed over some tears and uses implants, inserted endoscopically, to pull the obstructing prostate lobes away from the urethra. It has the advantage that it can be performed under local anaesthetic in an outpatient setting. Tom McNicholas, one of the founders of urolift, developed several of versions of it between 2004 to 2017 eventiually allowing it to become an accepted standard BPH treatment |
| 2013 onwards |
REZŪM ®
First described by Michael Hooey in Minnesota, and popularised in the UK by Richard Hindley and others. Rezūm uses pressurised steam to shrink the prostatic tissue with a very low risk to the patient, and good symptomatic relief |
|
2015
onwards
|
AQUABLATION
Robotic-assisted waterjet ablation was first described by Peter Gilling in New Zealand and has been popularised in the UK by Neil Barber and others |
Additional information
Click on any image below to access more detailed information about items & individuals featured above, or click here to go to the main History section of this website for more general history content:
|
Books on TURP
|
Harold Hopkins
|

John Blandy
|
|
The Thompson Punch
|
The Punch Club
|

Resectoscopes
|
|

Terence Millin
|

John Wickham & the "Probot"
|
|
← Back to BAUS 80th Anniversary