What does the prostate gland do?
The prostate gland lies just beneath the bladder and is normally about the size of a chestnut. The urethra (water pipe) runs through the middle of the prostate. The main function of the prostate is during your reproductive life. It produces fluid containing chemicals which nourish sperms to help with fertilisation.
What should I do if I have prostate symptoms?
If you have difficulty starting or stopping your urine flow, a weak stream, a feeling that you do not empty your bladder completely, increased frequency and urgency of urine passage by day or night and a tendency to dribble after you have finished, you should contact your GP for further advice
Your GP will normally review you initially and may supply you with the INternatinal Prostate Symotim Score (IPSS) and/or a bladder diary to complete before your appointment.
Download the IPSS Download a bladder diary
Referral to a urologist is only indicated if:
- your symptoms are severe;
- your urine flow is very poor;
- your blood tests (e.g. PSA) are abnormal; or
- there are any complications of the condition (e.g. chronic retention, urinary infection, bladder stones).
What are the facts about prostate symptoms?
- By the age of 65 years, 50% of men will experience benign enlargement of the prostate. At the age of 90, 90% of men have prostatic enlargement;
- An enlarged prostate alone does not always cause symptoms;
- The severity of the symptoms is not related to the size of the prostate;
- 1 in 3 men will suffer prostatic symptoms during their life;
- 1 in 10 men will require surgical treatment for their symptoms;
- Not all urinary symptoms in men are due to an enlarged prostate - incontinence, pain or blood in the urine may be due to other conditions;
- The risk of prostate cancer is not increased by having benign enlargement of the prostate. You are no more likely to develop prostate cancer than a man without benign prostatic enlargement;
- 30-40% of men with prostatic symptoms do not experience worsening of their condition with time and may not require any treatment;
- If treatment is indicated, this usually involves with drugs which relax the muscle in and around the prostate and/or drugs which shrink the glandular component of the prostate;
- If symptoms are severe, if there is no response to medical treatment or if there are complications of prostatic enlargement, surgical treatment may be indicated; and
- The risk of acute, painful retention of urine is small (approximately 1 in 100) and it is not always preceded by prostatic symptoms. Acute retention usually requires surgical treatment.
What should I expect when I visit my GP?
Your GP should work through a recommended scheme of assessment for men with prostatic symptoms. This will normally include some or all of the following:
1. A full history
Your GP will take a general history and a more detailed urological history. Using the symptom score and voiding dairy (see above), this will allow your GP to understand the severity of your symptoms and, in particular, how much they affect your daily activities. You may also be asked about your erections because reduced erections and prostatic symptoms often go together.
Some drugs can affect your bladder function and it is important that your GP is aware of all the drugs you are taking.
In younger men (less than 45), "prostate-like" symptoms are often due to other problems such as a stricture in the urethra (water pipe); Your GP will ask about previous injuries, diseases or operations in this area which may cause a stricture to develop.
2. A physical examination
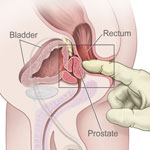 A full physical examination is normally performed, including measurement of your blood pressure. Your GP will usually perform a rectal examination (pictured) to assess the size and texture of the prostate gland.
A full physical examination is normally performed, including measurement of your blood pressure. Your GP will usually perform a rectal examination (pictured) to assess the size and texture of the prostate gland.
Your abdomen may also be examined to feel for an enlarged bladder.
If there is any suggestion that your symptoms are due to a neurological problem, your pelvic reflexes will normally be tested.
3. Additional tests
a. General blood tests
The actual blood tests performed will be left your your GP's discretion. It is essential to measure kidney function and to check the blood for anaemia or other problems.
b. PSA (prostate-specific antigen) measurement
It is usual to measure PSA levels in the blood in men with prostatic symptoms. If you are concerned about this, you should download and read the leaflet on PSA measurement ,and discuss the test with your GP.
Download the leaflet on PSA measurement
If your PSA is measured and is found to be raised above normal levels, or if your prostate feels abnormal on rectal examination, your GP will normally refer you urgently to see a urologist with a view to further tests to exclude prostate cancer.
Having a raised PSA does not mean you have prostate cancer. 50-60% of men with benign enlargement of the prostate have a raised PSA level. The only way to exclude prostate cancer is to see a urologist for further tests.
c. Urine tests
 Your urine will be tested for any abnormality and a sample will normally be sent to the laboratory to exclude infection.
Your urine will be tested for any abnormality and a sample will normally be sent to the laboratory to exclude infection.
d. Other specific tests
Other tests are not always necessary at this stage but your GP may wish to have a more detailed assessment by arranging:
These tests will normally be performed in the urology clinic if your GP feels that a referral is needed.
What could have caused my prostate to enlarge?
In general terms, we know very little about why the prostate gland enlarges with increasing age but hormone imbalance within the gland itself probably plays a part as well as certain genetic factors
There is some evidence that hormones and certain growth factors may work together to cause the prostate gland to enlarge. There also seems to be an inherited tendency in approximately 1 man in 10.
What treatments are available for this problem?
No treatment is likely to clear all your symptoms completely but they can be greatly improved so that the degree of "bother" is minimal; your symptoms can then be monitored regularly to see whether changes in treatment are needed
Treatment options include:
General measures ("watchful waiting")
If you and your GP decide treatment is not necessary initially, some simple, self-help measures can improve your quality of life:
- limit your fluid intake when you know you will be out of the house;
- try emptying your bladder twice each time by returning to the toilet after a few minutes for another attempt at emptying;
- reduce your caffeine, alcohol & nicotine intake, all of which cause you to make more urine;
- if you suffer from urgency, try distraction techniques (e.g. by using breathing exercises or counting) to take your mind off the urge to pass urine;
- if your stream is slow to start, try relaxation measures when standing to pass urine; and
- try "holding on" as long as possible to improve your bladder capacity.
Your symptoms may improve significantly with these measures. If they do not, you should go back to see your GP and get further advice.
Download a leaflet about self-help measures in men with lower urinary tract symptoms
Drugs
The drugs used for bladder outflow obstruction fall broadly into three main groups, shown below:
ALPHA-BLOCKERS (e.g. tamsulosin, terazosin, alfuzosin, doxazosin)
These drugs will normally be the first type of drug your GP prescribes. They relax the muscles in and around the prostate & bladder neck to make passing urine easier. Alpha-blockers may cause low blood pressure, a stuffy nose, skin rashes and impaired ejaculation. They (tamsulosin, in particular) should not be taken if you are scheduled to undergo cataract surgery, because they cause floppiness of the iris which can cause difficulties with the cataract surgery.
5-ALPHA-REDUCTASE INHIBITORS (e.g. finasteride, dutasteride)
These drugs shrink large prostate glands (glands greater than 40 grams) and may be used on their own (or together with alpha-blockers if your PSA is more than 1.5; see below*). They can cause impaired or low-volume ejaculation. They take up to 6 months to have maximum effect, and are less effective in men with smaller prostates. Importantly, they also reduce the PSA level in your blood by at least 50%.
PHOSPHODIESTERASE TYPE-5 INHIBITORS (PDE-5i, e.g. sildenafil, tadalafil, avenafil, vardenafil)
If, as is often the case, your symptoms of bladder outlet obstruction are associated with significant erectile dysfunction (impotence), you may benefit from treatment using one of the drugs that improves erections; these drugs may also have a beneficial effect on your prostate symptoms. They may cause headaches, indigestion, back pain, facial flushing and a stuffy nose.
With larger prostates, a combination of an alpha-blocker and a 5-alpha-reductase inhibitor has been shown to be more effective than either type used alone. The combination reduces the risk of complications from prostate obstruction (especially retention of urine), and may reduce the need for any subsequent prostate surgery.
Herbal Remedies
 Some herbal & plant extracts (e.g. saw palmetto; pictured right) are effective in relieving symptoms without the risk of significant side-effects. The extracts probably work because they contain plant hormones (very similar in structure to human hormones) that alter the hormone balance within the prostate. These extracts are not available on prescription from your GP, but can be purchased from reputable chemists and health food outlets. Side-effects from these plant extracts are very unusual.
Some herbal & plant extracts (e.g. saw palmetto; pictured right) are effective in relieving symptoms without the risk of significant side-effects. The extracts probably work because they contain plant hormones (very similar in structure to human hormones) that alter the hormone balance within the prostate. These extracts are not available on prescription from your GP, but can be purchased from reputable chemists and health food outlets. Side-effects from these plant extracts are very unusual.
Surgery
Surgical treatment is usually recommended if symptoms are severe, if medical treatment has failed, or if the side-effects of other treatment are not tolerated or undesirable.
The main surgical options are outlined in the table below (with links to documents containing more detailed information about risks & benefits):
Transurethral resection of the prostate (TURP)
Removal of the central, obstructing part of your prostate, using a wire loop and electric cautery, through a telescope passed along your urethra (waterpipe)
Green light laser prostatectomy (GLLP)
Removal of the central, obstructing part of your prostate, using a wire loop and electric cautery, through a telescope passed along your urethra (waterpipe)
Holmium laser enucleation of the prostate (HoLEP)
“Peeling out” the central obstructing part of your prostate gland using a laser fibre, through a telescope passed along your urethra
Rezūm steam ablation
Injecting puffs of steam into your enlarged prostate, using a specially-designed instrument passed along your urethra, resulting in shrinkage of your prostate
Urolift ™
Inserting special implants into your urethra to pull back the obstructing prostate tissue and improve your urine flow
Prostate artery embolisation (PAE)
A technique where an expert radiologist (X-ray doctor) blocks off the arteries to your prostate gland, causing it to shrink over time. This does not involve surgery but a highly skilled technique known as "interventional radiology"
Bladder neck incision (sometimes called a prostatotomy)
Sometimes, when the prostate is small, we can simply cut the muscle at the neck of your bladder telescopically without actually removing the prostate. Usually, your surgeon can only decide if this is appropriate after looking inside your bladder
Open or laparoscopic simple prostatectomy
Removal of the obstructing prostate tissue, either through a surgical incision in your lower abdomen (tummy) or using a laparoscopic (keyhole) technique, especially when your prostate is very enlarged
Catheterisation of your bladder
Permanent catheterisation
This may be used in patients who, for one reason or another, are not considered suitable for surgery; the catheter may be put into your bladder through your penis (an urethral catheter), or through a small incision through the skin just above your pubic bone (a suprapubic catheter)
Intermittent self-catheterisation
This involves passing a disposable catheter yourself into your bladder, through your urethra, to drain it. It is an alternative to permanent catheterisation (see above) for men who cannot pass urine and are not considered suitable for surgery, but does require a significant degree of manual dexterity
Page dated: March 2024 - Due for review: August 2026