Trainees
Diagnostic Pathways in Suspected Renal Colic
 This is a retrospective audit of local diagnostic pathways in patients presenting with suspected ureteric colic. It looks specifically at the time taken to perform a CT KUB, whether appropriate laboratory investigations are requested and whether the recommended analgesia is prescribed.
This is a retrospective audit of local diagnostic pathways in patients presenting with suspected ureteric colic. It looks specifically at the time taken to perform a CT KUB, whether appropriate laboratory investigations are requested and whether the recommended analgesia is prescribed.
Backgroud to the audit
Ureteric colic is a common condition which causes significant morbidity and socio-economic burden for both patient and healthcare provider. Prompt diagnosis and symptom control aims to improve the patient experience and facilitate treatment as required.
Both BAUS and NICE have produced similar guidance which forms the audit standards below.
The standard
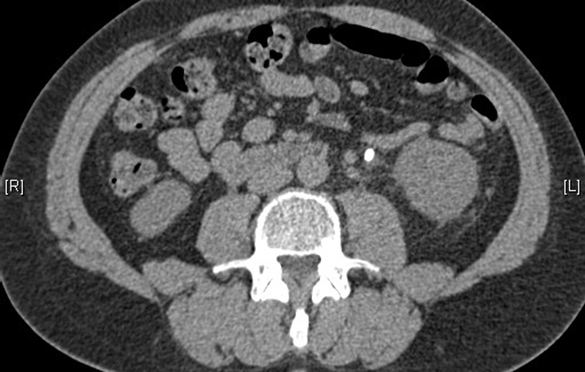
A non-contrast CT KUB should be performed within 14 hours (BAUS) for the standard (non-pregnant adult). 24 hours may be considered acceptable (as per NICE guidance), particularly in centres not routinely offering out of hours imaging.
Investigations in all patients should include serum calcium and urate (BAUS).
Non-steroidal anti-inflammatory drugs (NSAIDs) should be given as first-line analgesia (unless contra-indicated) (BAUS / NICE). Intravenous paracetamol should be offered if NSAIDs are contra-indicated or not effective (NICE).
Assessment of local practice
Perform a retrospective review of consecutive patients with suspected ureteric colic who had CT KUB.
Data items to be collected
-
patient demographics
-
date and time CT KUB requested
-
date and time CT KUB performed
-
positive CT KUB (ie. confirming ureteric calculi)
-
serum calcium and urate measured
-
NSAIDs (or other form of analgesia) prescribed (on admission / to take home)
Suggested nunbers
100 consecutive patients.
Estimated time required
10 hours.
Suggestion(s) for change if targets are not met (* see below)
-
Consider creating or updating a trust pro-forma in conjunction with A&E and radiology giving advice on the initial investigation and diagnosis of ureteric colic
-
Present in local audit meeting / departmental teaching sessions (to A&E, radiology and pharmacy) and discuss areas for improvement
-
Consider any barriers to compliance e.g.
-
Outsourcing of imaging services, especially overnight or at weekend
-
Difficulty contacting patients who have been sent home to await a scan appointment
- Re-audit following improvements
(* please consider if any other improvements are possible, even if all targets have been met)
Further work
Once a cohort of patients has been identified you may wish to audit their subsequent management, as per the BAUS and NICE guidance (eg. offer ESWL or primary URS within 48 hours). Most centres will struggle to achieve this standard.
Consider barriers and ways this could be improved at your centre (eg. access to emergency theatre / on-site lithotripsy).
Publication & contact details
Published Aug 2019 - Miss Rashmi Singh, Kingston NHS Foundation Trust, London and Mr Andrew Brown, CT2 (email the author).
← Back to essential audits