What should I do if I have male menopause symptoms?
If you have any combination of the symptoms below, you should seek further advice from your GP
What are the facts about the male menopause?
The preferred term for the male menopause (sometimes called the andropause) is Androgen Deficiency in the Ageing Male (ADAM). The symptoms of ADAM are non-specific and may include:
- alterations in the circulatory & nervous systems (hot flushes, sweating, insomnia & nervousness);
- changes in mood and mental function (anxiety, irritability, poor sleep, constant tiredness, poor short-term memory & low self-esteem);
- changes in virility (decreased physical energy, decreased muscle strength & inability to participate in sporting activities);
- diminished sexual function (reduced sex drive, poor erections & impaired ejaculation);
- changes in physical appearance (abdominal weight gain, loss of body hair, diminished muscle mass & loss of height); and
- changes in body metabolism & chemistry (increased LDL cholesterol, increased total body fat, osteoporosis & reduction in the red blood cells in the blood).
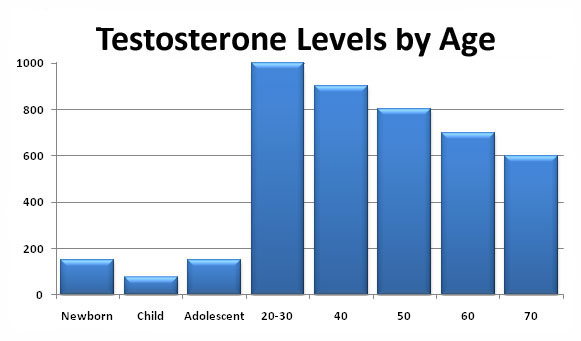
The common factor which lies behind these symptoms is a reduction in the levels of active testosterone (male hormone) in the blood with increasing age:
At the same time, there is an increased risk of heart disease, obesity, high blood pressure and diabetes. All of these can contribute to health problems. The overall picture associated with ADAM is, therefore, very complex.
What should I expect when I visit my GP?
Your GP should work through a recommended scheme of assessment for men with symptoms of the male menopause. This will normally include one or all of the following:
A full history
Your GP will take a full history, concentrating on all the symptoms mentioned above, and will also ask about "lifestyle" factors (stress, physical activity, smoking habits, alcohol consumption & drug consumption).
A physical examination
A full physical examination will normally be performed including rectal examination of the prostate gland and measurement of your blood pressure.
Additional tests
The usual tests performed are:
a. General blood tests
Your GP will decide which tests to perform. These will normally include measurements of kidney, liver, bone & thyroid function, a blood sugar and cholesterol measurement as well as a check on your blood cells for anaemia and other problems
b. Hormone measurements
Your testosterone levels will be measured with your sex hormone-binding globulin (SHBG). This will allow your GP to see how much active (free) testosterone is in your bloodstream. Follicle cell stimulating hormone (FSH), luteinising hormone (LH) and prolactin levels, which control testosterone production by the testicles, may also be measured.
c. Other specific tests
Your GP may check your body mass index (BMI) using your height & weight. An ECG or bone density measurement (to look for osteoporosis) may also be arranged. Your PSA will be checked, especially if you are over 50, to test for possible prostate cancer. Finding cancer would prevent you from taking testosterone replacement therapy (TRT).
Download information about having your PSA checked
If you are less than 50-years-old with symptoms of ADAM, it is normally recommended that you have a detailed hormone assessment with a hospital endocrinologist to exclude an underlying hormone problem.
What could have caused my menopausal symptoms?
ADAM is caused by a reduction in active (free) testosterone levels but why this causes such diverse symptoms is not clear
Testosterone is made predominantly by the testicles. They are stimulated to produce it by other circulating hormones which originate from the pituitary gland at the base of the brain. Testosterone deficiency is probably due to an imbalance in the hypothalamic-pituitary-testicular axis.
It is not known why testosterone levels fall with increasing age or why active testosterone deficiency results in such a wide variety of symptoms. Low levels of active (free) testosterone may occur if SHBG levels are raised. This can happen in heavy drinkers, in men who smoke more than 10 cigarettes a day and in men with an underactive thyroid gland.
What treatments are available for this condition?
If you have significant symptoms and reduced blood levels of active testosterone, testosterone replacement therapy (TRT) should be considered
General advice
Your GP will advise you about modification of your lifestyle by finding new ways to relieve stress, eating a healthy diet, getting plenty of sleep, exercising regularly, limiting your intake of alcohol and stopping smoking. If your symptoms are particularly troublesome, and not helped by general measures, your GP may then consider hormone replacement.
Testosterone-replacement therapy (TRT)
TRT should be considered, when symptoms are present and testosterone levels are low, for:
- men with sexual dysfunction i.e. erectile dysfunction (impotence), loss of spontaneous erections or low sexual desire (loss of libido);
- men with type 2 diabetes;
- men who are overweight with a BMI greater than 30, or waist circumference more than 102 cm (40 inches);
- men at risk of side-effects from opioids, antipsychotics or anti-epileptic drugs.
TRT may be given by tablets, injections, gel or patches; most men find the last two more convenient. The risk of cardiovascular disease should be assessed before, and monitored during, treatment. Blood levels of testosterone need to be measured regularly to ensure that they are kept within the normal range.
Side-effects
TRT is unlikely to cause prostate cancer, and there is no evidence that it is unsafe if you have localised, low-risk prostate cancer. It can, however, cause enlargement of a benign prostate gland and this may result in troublesome symptoms. You should have regular PSA (prostate-specific antigen) tests and rectal examinations to monitor your prostate gland if you do have prostatic symptoms.
Cholesterol and red blood cells levels may also be affected by TRT, and should be closely monitored. You may notice headaches, weight gain, acne and worsening baldness whilst taking TRT. It is important to note that, whilst your troublesome symptoms may improve, the long-term benefits of TRT treatment are not accurately known.
TRT should not be prescribed if you have certain medical problems, so please inform your GP if you suffer from any of the following conditions:
- known breast cancer or high-risk (advanced) prostate cancer;
- thick blood or "sticky" red blood cells (hyperviscosity syndromes);
- high red blood cell count (packed cell volume greater than 50%);
- untreated obstructive sleep apnoea;
- severe prostatic symptoms; or
- class III or IV heart failure.
European guidelines on testosterone deficiency
PDE-5 inhibitors
TRT alone may improve your erections but this is not guaranteed. If erectile function remains a problem during TRT treatment, ask your GP to consider prescribing Viagra (sildenafil), Cialis (tadalafil), Levitra (vardenafil) or Spedra (avanafil) as well.
Information about PDE-5 inhibitors
Page dated: March 2024 - Due for review: August 2026